Barton Malow is constantly working towards finding the most effective and efficient ways to serve our clients’ growing needs through innovation, technology, and continuous improvement. Learn more about where we came from, what we’re doing, and where we’re going next.
Building with the American Spirit People Projects Communities

100 years of operation Explore Our History
3.5K Team Members Across North America Work With Us
111M Hours Worked in 5 years View Our Safety Commitment

Projects
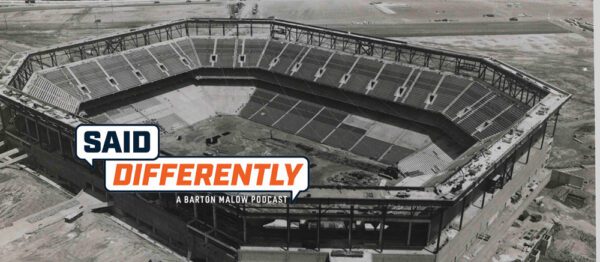
New Said Differently: Listen to ‘Under Pressure: Raising the Roof on the Pontiac Silverdome’
April 24, 2024 2 minute read
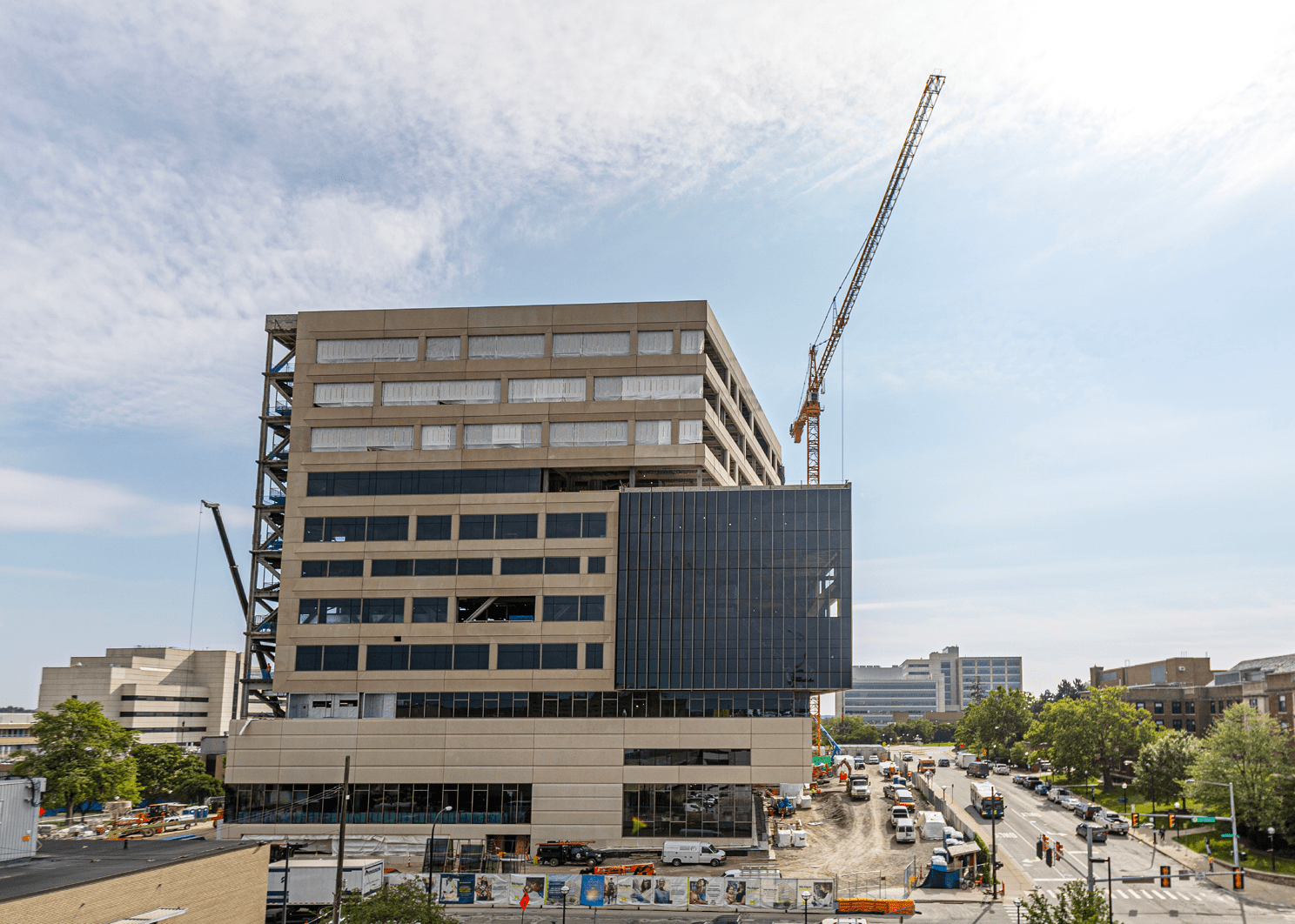
Projects
Hudson’s Site Construction Reaches New Heights
April 11, 2024 4 minute read
People
Women in Construction: Transforming the Business
March 13, 2024 1 minute read
Communities
Piedmont Concrete Contractors is Laying Central Virginia’s Foundation
March 7, 2024 5 minute read
People
Listen to ‘Said Differently – Beyond the Build: Kim Hoffman’ Now
March 5, 2024 1 minute read
People